Eye Related Disease
Jump To
Clinical Signs of Graves’ Disease
Graves’ disease can be associated with many clinical symptoms. The most obvious sign is bulging eyes, or exophthalmos. This can present with edema, thickening of the skin usually found on the lower extremities, fatigue, weight loss with increased appetite, rapid heartbeat and muscular weakness.
Graves’ disease is the most common cause of diffuse goiter. A large goiter (thyroid gland ) may be visible, but a smaller goiter may only be clinically determined. Hyperthyroidism, i.e., overproduction of the thyroid hormones T3 and T4, is another sign of Graves’ disease. Normothyroidism is also seen along with hypothyroidism, which may cause goiter.
Specifically related to the eye, Graves’ disease may be marked by eye pain, irritation, tingling sensation behind the eyes, or the feeling of sand in the eyes. In addition, eye swelling/redness or eyelids/eyelid retraction may be experienced along with sensitivity to light.
Before & After Photos
Additional symptoms related to Graves’ disease may include: palpitations, tachycardia (100-120 beats per minute, or higher), arrhythmia, hypertension, tremor, excessive sweating, heat intolerance, increased appetite, unexplained weight loss, decrease in appetite, shortness of breath, muscle weakness, insomnia, change in sex drive, increased energy, fatigue, mental impairment and memory lapse, anxiety, irritability, restlessness, erratic behavior, brittle nails, abnormal menstrual cycles, difficulty conceiving, chronic sinus infections, diarrhea, panic attacks, and/or abnormal breast enlargement.
Eye Disease
Thyroid-associated ophthalmopathy is a common symptom of Graves’ disease. Thyroid eye disease is an inflammatory condition that affects the orbital contents along with the extraocular muscles and orbital fat. These conditions may also be observed in Hashimoto’s thyroiditis, primary hypothyroidism, or thyroid cancer.
The ocular symptoms particular to Grave’s disease include soft tissue inflammation, unilateral or bilateral protrusion, corneal exposure, and optic nerve compression. More general symptoms associated with hyperthyroidism include lid retraction, lid lag, and a delay in downward gaze of the upper eyelid.
Graves Disease
Graves’ disease commonly causes proptosis in adults between the ages of 25-50. Diagnosis is based on clinical findings including proptosis, eyelid retraction, restrictive myopathy, and/or compressive optic neuropathy. It is often grouped into Type I and Type II orbitapathy.
More Frequent Signs:
More frequent signs of Graves’ disease include: lid lag of the upper and lower lids, exophthalmos, diplopia, and/or lid edema.
Less Frequent Signs:
Less frequent signs of Graves’ disease include: closed lid tremor, infrequent blinking, decrease forehead wrinkling with upgaze, increased pupil size fluctuation, and/or pigmented lids.
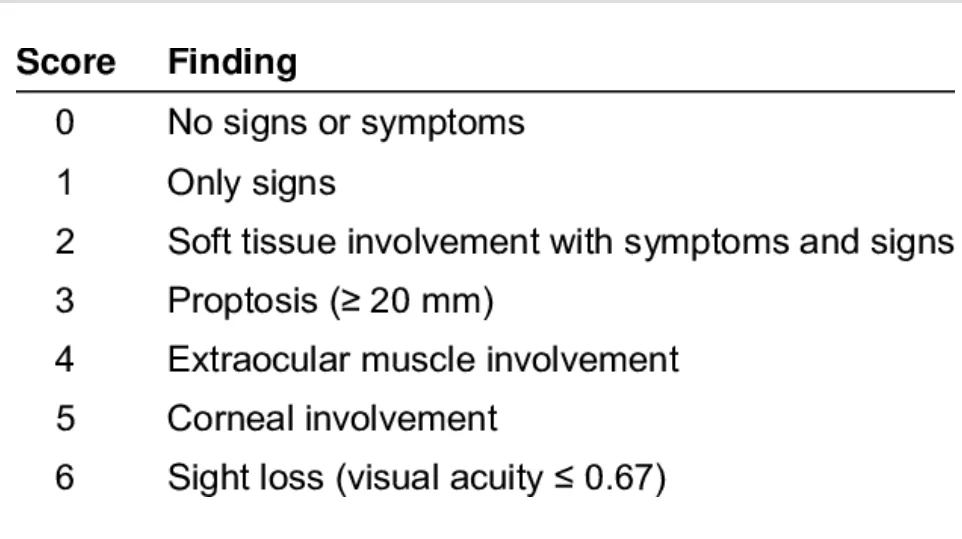
Werner’s Classification
Werner’s classification grades only the clinical severity of Graves’ ophthalmology.
Clinical findings assist in diagnosis and may be confirmed using a CT scan to show enlargement of multiple extraocular muscles, most commonly the inferior and medial rectus.
Treatment for systemic thyroid disease (hyperthyroid, hypothyroid, or euthyroid) may include topical lubrication, systemic steroids, orbital decompression surgery, extraocular muscle adjustment, eyelid recession surgery, and/or radiation therapy.